Meet Patricia, a sharp and thoughtful lady of 65. For more than a decade, her bone density had been declining steadily. In 2017, she was diagnosed with osteoporosis and her doctor gave her 2 options. Either try a new type of medication or strength training. Having been on medication for years with no results to show for, she had enough of taking pills and decided to go with strength training.
Patricia deadlifting 30kgs when she first started training.
3 years later, she deadlifted 110kgs
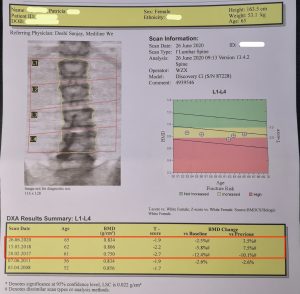
After training with us for 3 years, Patricia has gotten way stronger. Her most recent bone scan showed that she is out of osteoporosis range. A few months back, she was at home barefooted and running towards the kitchen. The lights weren’t turn on and she didn’t realise a few ice cubes had dropped on the kitchen floor earlier and melted. As she was approaching the kitchen, she stepped on the puddle of water, slipped and fell. Being strong with denser bones, she managed to catch herself from falling flat onto the floor. Thereafter, she simply stood up and carried on, totally unscathed.
However, if the same thing happened to her friends, many would not be okay.
Falling is a common problem in an aging population
Patricia shared with us that she knows of a number of older adults who have had falls over the last few months. None of them got up as easily as she did. Most suffered from some form of injury, and some injuries were quite severe. An acquaintance fell and broke a bone in her hand. Her friend’s mother fell and is currently hospitalised with bleeding in the brain.
According to the Health Promotion Board, about one-third of elderly Singaporeans aged 60 and above have fallen at least once. For an elderly person, falls are dangerous because they can cause hip fractures. Women have an 18% chance of getting a hip fracture in their lifetime, while for men it is 6%. The risk of hip fracture is even higher in people diagnosed with osteoporosis.
Hip fractures have dangerous consequences for the elderly
According to the American Academy of Orthopaedic Surgeons:
- 20% of elderly hip fracture patients die within 1 year after their fall
- 50% become dependent on a cane or walker
- 40% will need to be admitted to a nursing home, because they cannot perform daily activities like eating, bathing, getting dressed and going to the toilet
- Only 25% of older adults who suffer a hip fracture from a fall actually make a complete recovery
Aside from physical injuries, falls in the elderly can also have a psychological impact, such as:
- Loss of autonomy and confidence when they become dependent on help to get around
- Developing a fear of falling that could lead to withdrawal from social activities
- Loneliness and ultimately, depression
The elderly face many risk factors for falling down
Why do the elderly fall? Common risk factors include:
- Environmental and safety hazards
- Existing medical conditions
- Medications that can cause dizziness
- Poor vision
- Joint problems and general muscle weakness
- Poor balance and slow reaction time
Of the above, many are out of your control, like the environment outside of your house. Or, they require specific medical therapies and treatments, often with additional complications. The exceptions are muscle weakness and poor balance – these factors can be improved with training and are entirely in your hands.
Also, while there are many reasons why you might lose your balance, you don’t actually have to fall. If you can get your center of mass back over your base of support, you won’t fall. Your center of mass is a reference point representing the averaged mass of an object in space – for humans like you and I standing in the anatomical position, this point would roughly be somewhere a couple of centimeters in front of your sacrum. Note that this is not a static point and can change position depending on the person’s shape, position or by the addition of an external load. The other component is your base of support – for humans like you and I standing in the anatomical position, this is located at midfoot. Its position, like with the center of mass, can also change with movement.
For balance to be maintained, muscular force is required to overcome overbalancing as a result of your center of mass not being positioned directly over your base of support. Strength is required to overcome overbalancing and to maintain it. Let’s see how this works.
Fall prevention is about improving strength
What actually happens when you fall? Let’s look at it in slow motion. First you lose your balance, then you flail around trying to catch yourself, but usually you fail to regain your balance, and before you know it, you’re on the ground.
Most of the time, when the elderly fall, the issue is not the lack of balance itself, but rather the inability to regain their balance after they’ve lost it. In other words, they’re not strong enough to catch themselves when they lose their balance.
Remember the last time you stepped on something and slipped while you were walking? Try to remember exactly what you did so that you didn’t fall. If you didn’t fall, it was because you managed to catch yourself an exert enough force to move your center of mass back over your base of support. Now imagine that if you couldn’t do that because you weren’t strong enough – you’ll end up on the floor.
So strength actually helps to prevent falls. The ability to stay in balance is a function of being strong enough.
Sometimes you can’t avoid slipping or tripping over something – these things happen. You don’t see a small curb on the pavement or you stepped in a little puddle of water and slip. What matters is that regardless of the situation you’re in, you have the ability to save yourself. I believe it is better to work on yourself, so that you are strong enough to regain your balance after you’ve lost it.
Balance training versus strength training
In recent years, “balance training” has become quite popular to combat the fear of falling. In general, balance training tries to improve your balance through “unstable surface” exercises. The idea is that if you can train yourself to stand on a rubber ball, or on one foot, you should find it easier to stabilise yourself on flat ground, and therefore decrease the risk of falling.
But this is the wrong thinking. This sort of training doesn’t help when you actually fall. Trying to improve your balance by doing “balance training” doesn’t translate over to day to day living because first of all, you can’t get strong doing these exercises. Strength is important is maintaining balance, remember? The second problem is that unless you’re in the Cirque du Soleil, you spend your days walking around on firm, stable ground. Since you don’t walk around on unstable surfaces, what’s the point of “training” on an *insert unstable balance training equipment here*.
Remember the slow-motion fall described above? Every fall starts by overbalancing. Muscular strength is needed to counteract that overbalancing, in other words, to interrupt that falling action and get your center of mass back over your base of support. The reason most people complete the fall is because they are weak, and don’t have enough strength to restore their balance.
So the best way to improve balance is actually strength training, to increase the muscular force needed for maintaining balance.
Barbell strength training increases bone density
For older people, especially those with osteoporosis, the most efficient form of training is strength training, specifically barbell strength training. Read more about why barbell training works the best here and here. It not only gets you stronger to better regain balance, it also increases your bone density; so in the event that you’re unable to save yourself from falling, your bones will be more resilient to fractures.
If you have no experience with gyms, equipment like barbells can seem intimidating and we understand that. Why not just do basic strength exercises that use your body weight, like push-ups and lunges?
You may think that these exercises are enough to build strength. But actually, the main driver of increased strength and bone density is incremental external loading—this means using external weights. While some strength training is better than none, bodyweight exercises very quickly reach their limitations. For building strength, you need external loading, and nothing works better than barbell training.
At Hygieia Strength & Conditioning, older folks like yourself start out with the Novice Linear Progression (NLP), a simple but systematic strength training program. Of course, we understand that not everyone will be able to follow this program as laid out – modifications to the lifting techniques or programming can be made to accommodate any limitations or special conditions you may have. Find out more about how older clients train with us.
Strength training can naturally reverse osteoporosis
These days, Patricia no longer has osteoporosis. She feels stronger and more confident, and is enjoying her active life. With the physical function and mobility of someone much younger, she is the envy of her friends.
She says, “Although I started barbell training with the goal of improving my bone density, I found that as I got stronger my balance improved as well. This is not so surprising. But what surprised me is the number of my friends or acquaintances who have injuries from falls. I hadn’t realised how common this is for folks in their 50s, 60s and beyond. Now I’m motivated to continue investing in my “strength bank” to build both balance and bone density.”
We did a video interview with Patricia, where she talks about her osteoporosis diagnosis and beating it with barbell strength training. In another video, she shows us how she trains.
Your mindset that it’s too late to do something about your strength and bone loss need to change. It’s never too late. If you’re older and with fragile bones, acting earlier is always better than later. You need to focus on getting strong in the most efficient way possible, now.